In a recent HSJ article Dr Steve Kell, co-chair of NHS Clinical Commissioners, described five ways CCGs could progress their role in leading health service transformation. He included a call for better tools to further support intelligent commissioning.
Better intelligence is always useful, but it can only do so much. Motorists who monitor their tyre pressure will know that no matter how sophisticated the measuring equipment when a tyre is flat or losing pressure, it has to be changed. CCGs should be using the data they already have and acting on it, rather than waiting until the tools evolve to perfection.
CCGs already have access to a wide range of performance metrics they should be acting on. For example, current monthly SUS data can support a wealth of performance measures to address unwarranted variation in primary and secondary care across key areas such as service efficiency, financial sustainability and the quality of care.
New to follow-up outpatients appointments
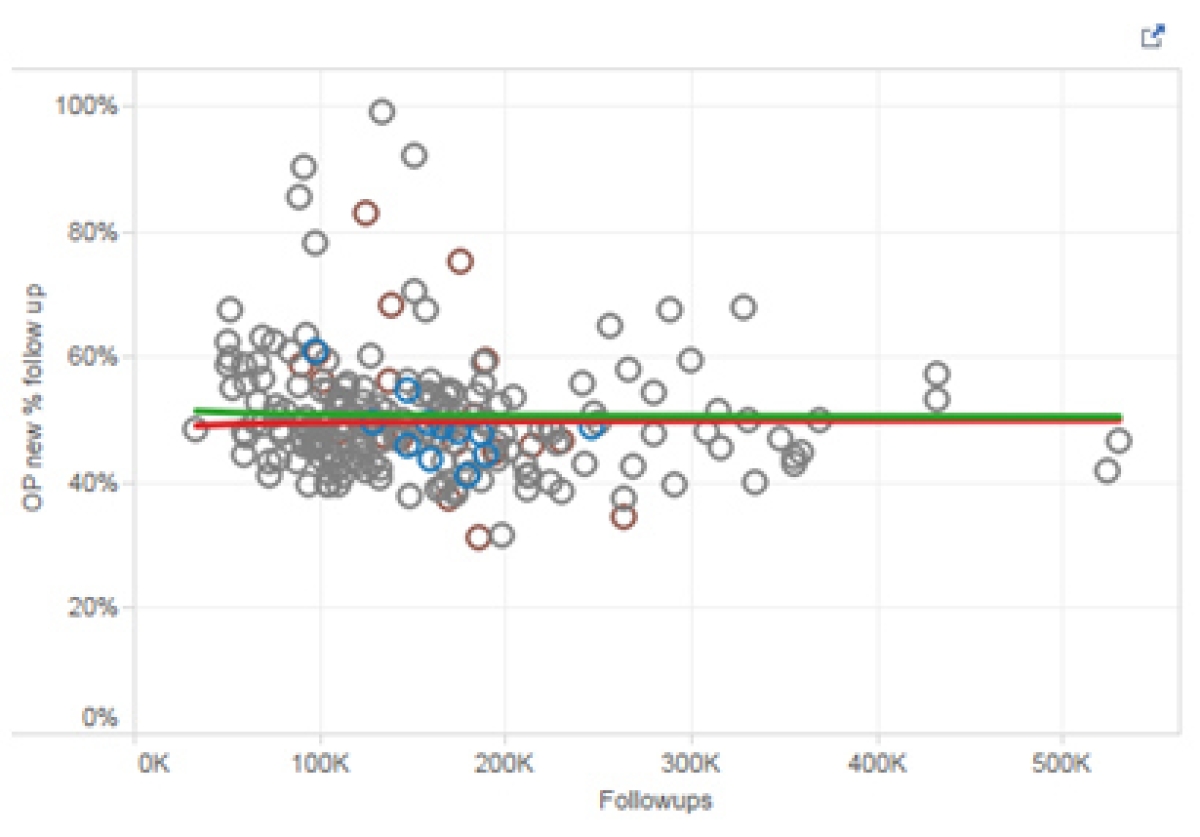
Transforming the interface of care between primary and secondary providers is critical to improving patient experience as well as reducing expenditure. New to follow-up outpatient appointments is where unwarranted variation thrives and can be identified with existing information.
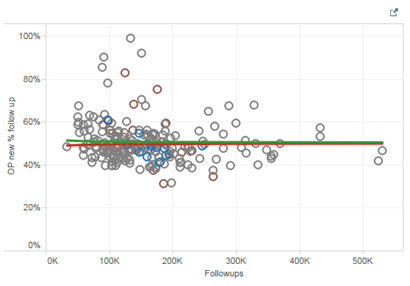
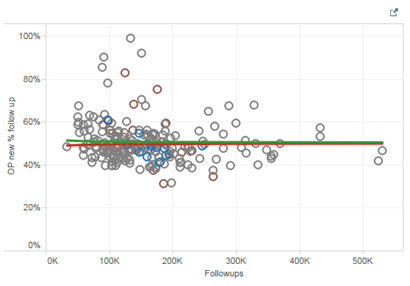
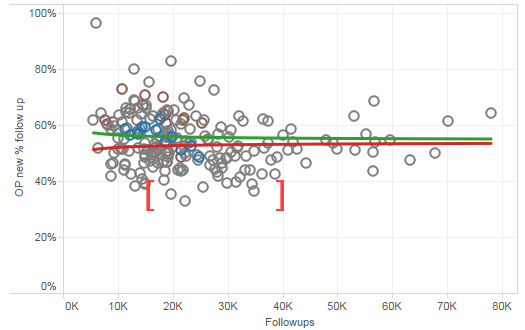
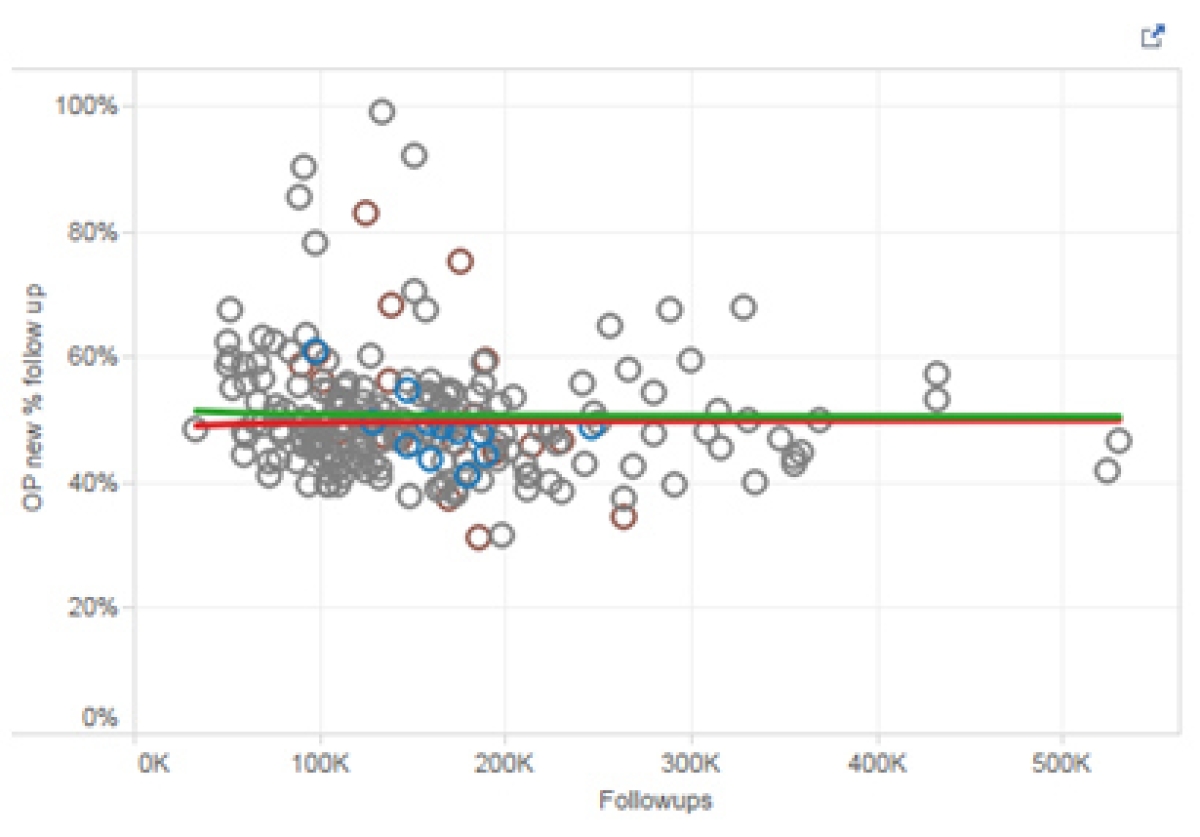
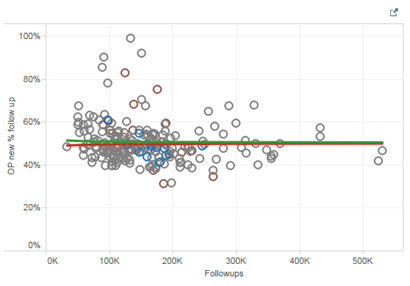
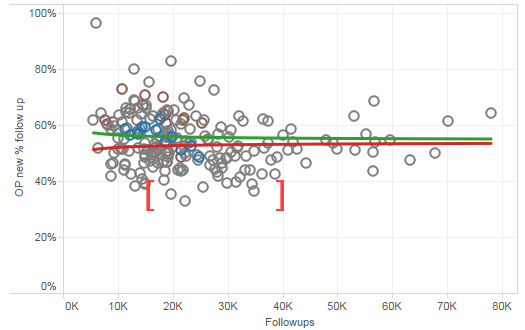
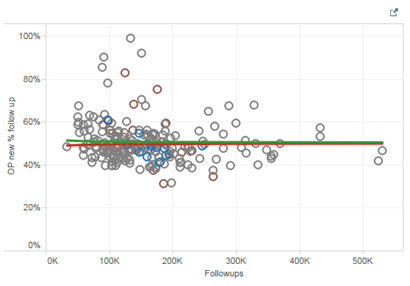
We took nationally-available data from HSCIC for the last financial year and applied this to all new to follow-up activity for every CCG to show how wide the variation is. Our analysis also reveals how much is statistically significant as it falls outside the upper (Green) and lower (Red) confidence intervals in the graph below.
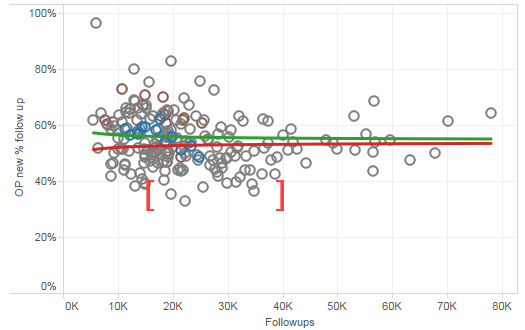
While a wide variation at this scale would be expected due to case mix and other confounding factors these are accounted for when we look at a single department (T&O) as illustrated below:
Here we see a clear significant positive unwarranted variation in reduction of new to follow-ups for several CCGs compared to their peers indicating they have a very different process to the others which probably involves a more primary care led management of these patients.
Management of patients with long term conditions in primary care
We know that closer monitoring and management of patients with long-term conditions in primary care is essential to prevent escalation of their care to the acute sector. Here they are at risk of further complication and there is a likelihood of a greater financial impact. It is therefore important for CCGs to track any unwarranted variation.
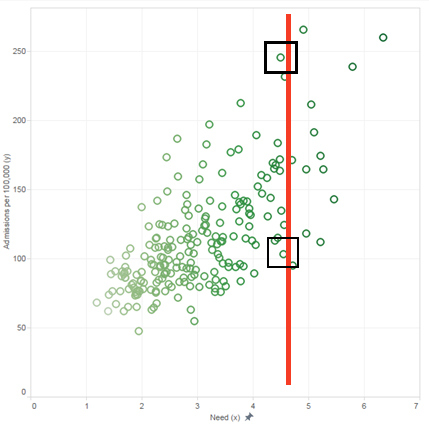
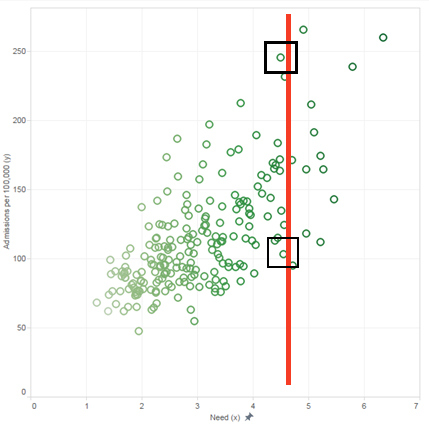
Using the same data source from the example above we looked at a population adjusted rate of emergency admissions for asthma using prevalence based on age and deprivation. In this example, where confounding factors had been accounted for, a low level unwarranted variation across CCGs would be expected but the chart below shows this is not the case.
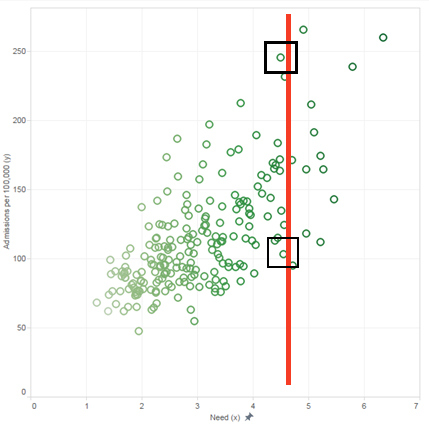
The red line represents a cluster point of CCGs whose prevalence profiles (need index) are similar to each other so are a true like for like comparison of variation.
Using this group we can see that the rate per 100,000 of population for emergency admission ranges from 103 to 245 or an unwarranted variation of 240 per cent within these CCGs. This is a large spread which will have a significant impact on the quality of care for patients as well as creating further stress on secondary care and its associated costs.
These two examples show there is a lot that can be done with existing data to address the significant unwarranted variation that exists across the system. What seems to be lacking is leadership to drive its use and act on it. This may be because CCGs do not realise this type of information is available, or simply not having the resources to undertake the analysis required to produce it in the first place.
Whatever the reasons, CCGs should embrace the intelligence they have now while they wait for the next generation of intelligence tools they aspire to be developed.
Paul Fitzsimmons, Sales and Marketing Director, CHKS
Our analysis contains HES data which is re-used with the permission of The Health & Social Care Information Centre. All rights reserved.In a recent HSJ article Dr Steve Kell, co-chair of NHS Clinical Commissioners, described five ways CCGs could progress their role in leading health service transformation. He included a call for better tools to further support intelligent commissioning.
Better intelligence is always useful, but it can only do so much. Motorists who monitor their tyre pressure will know that no matter how sophisticated the measuring equipment when a tyre is flat or losing pressure, it has to be changed. CCGs should be using the data they already have and acting on it, rather than waiting until the tools evolve to perfection.
CCGs already have access to a wide range of performance metrics they should be acting on. For example, current monthly SUS data can support a wealth of performance measures to address unwarranted variation in primary and secondary care across key areas such as service efficiency, financial sustainability and the quality of care.
New to follow-up outpatients appointments
Transforming the interface of care between primary and secondary providers is critical to improving patient experience as well as reducing expenditure. New to follow-up outpatient appointments is where unwarranted variation thrives and can be identified with existing information.
We took nationally-available data from HSCIC for the last financial year and applied this to all new to follow-up activity for every CCG to show how wide the variation is. Our analysis also reveals how much is statistically significant as it falls outside the upper (Green) and lower (Red) confidence intervals in the graph below.
While a wide variation at this scale would be expected due to case mix and other confounding factors these are accounted for when we look at a single department (T&O) as illustrated below:
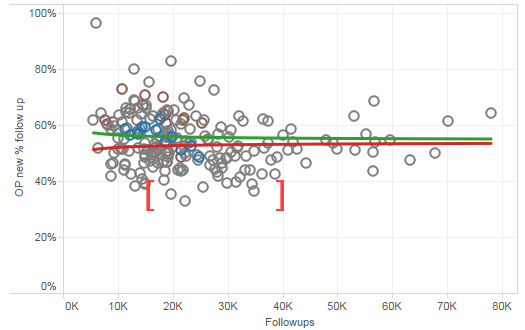
Here we see a clear significant positive unwarranted variation in reduction of new to follow-ups for several CCGs compared to their peers indicating they have a very different process to the others which probably involves a more primary care led management of these patients.
Management of patients with long term conditions in primary care
We know that closer monitoring and management of patients with long-term conditions in primary care is essential to prevent escalation of their care to the acute sector. Here they are at risk of further complication and there is a likelihood of a greater financial impact. It is therefore important for CCGs to track any unwarranted variation.
Using the same data source from the example above we looked at a population adjusted rate of emergency admissions for asthma using prevalence based on age and deprivation. In this example, where confounding factors had been accounted for, a low level unwarranted variation across CCGs would be expected but the chart below shows this is not the case.
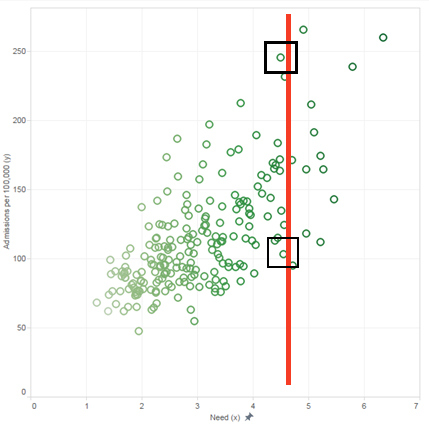
The red line represents a cluster point of CCGs whose prevalence profiles (need index) are similar to each other so are a true like for like comparison of variation.
Using this group we can see that the rate per 100,000 of population for emergency admission ranges from 103 to 245 or an unwarranted variation of 240 per cent within these CCGs. This is a large spread which will have a significant impact on the quality of care for patients as well as creating further stress on secondary care and its associated costs.
These two examples show there is a lot that can be done with existing data to address the significant unwarranted variation that exists across the system. What seems to be lacking is leadership to drive its use and act on it. This may be because CCGs do not realise this type of information is available, or simply not having the resources to undertake the analysis required to produce it in the first place.
Whatever the reasons, CCGs should embrace the intelligence they have now while they wait for the next generation of intelligence tools they aspire to be developed.
Paul Fitzsimmons, Sales and Marketing Director, CHKS
Our analysis contains HES data which is re-used with the permission of The Health & Social Care Information Centre. All rights reserved.In a recent HSJ article Dr Steve Kell, co-chair of NHS Clinical Commissioners, described five ways CCGs could progress their role in leading health service transformation. He included a call for better tools to further support intelligent commissioning.
 In a recent HSJ article Dr Steve Kell, co-chair of NHS Clinical Commissioners, described five ways CCGs could progress their role in leading health service transformation. He included a call for better tools to further support intelligent commissioning.
In a recent HSJ article Dr Steve Kell, co-chair of NHS Clinical Commissioners, described five ways CCGs could progress their role in leading health service transformation. He included a call for better tools to further support intelligent commissioning.